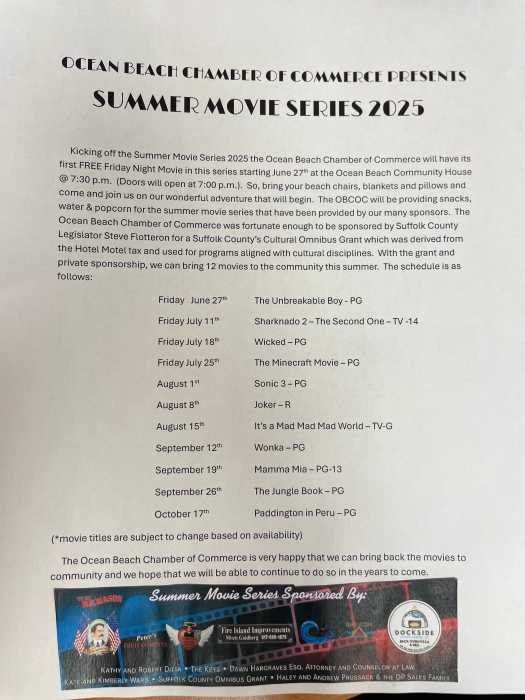
In 90-degree heat, 300 volunteer “patients” and more than a hundred SUNY Downstate Medical Center clinical and support staff and administrators participated in a Sunday morning disaster drill to test hospital response to a potentially life-threatening illness associated with cold weather — influenza.
“Although increasing numbers of people are vaccinated against flu every year, the emergence of new resistant stains of the virus that causes this disease is an ongoing reality. So, the potential of a flu epidemic requires that we be ready to handle a surge of patients with this extremely infectious disease,” said Bonnie Arquilla, DO, FACEP, director of disaster preparedness and assistant professor of emergency medicine at SUNY Downstate. Dr. Arquilla said that while the devastating 1918 influenza epidemic seems part of the distant past, the much more recent outbreak of Severe Acute Respiratory Syndrome (SARS) in China and of West Nile disease here caused world-wide awareness of the need to have medical response systems in place.
The disaster drill — called “Cover Your Cough 2008” — was planned and conducted by the New York Institute for All Hazard Preparedness (NYIAHP) with the New York City Department of Health and Mental Hygiene. NYIAHP includes representatives of SUNY Downstate, Kings County Hospital Center, Kingsboro Psychiatric Center, and Kingsbrook Jewish Medical Center.
The event was also supported by the Community Health Care Association of New York State, Emergency Medical Services, the New York Police Department, Office of Emergency Management, and New York Fire Department. Representatives of all SUNY Downstate hospital departments and administration were involved. Components of the drill were carried out at all participating hospitals.
Volunteer “patients” of every age arrived at Downstate, 450 Clarkson Avenue, at 9 a.m. They attended an orientation session and were briefed about the list of symptoms each “patient” was expected to present to screening clinicians. Volunteers were assured that they would not experience any real examinations.
While volunteers were being prepped, key hospital leaders representing areas including Infectious Diseases, Critical Care, Inpatient Services, Logistics, Maternal-Child Care, and many other services met and reviewed readiness in terms of available beds and stretchers, stock of isolation gowns, and specialized masks.
The exercise testing mass screening, isolation, and triage protocols began about 10 a.m. under a tent at the entrance to Downstate’s University Hospital of Brooklyn Emergency Department and at other facilities. Access for real emergencies was separated from the drill activities. “Patients” were first screened and each received a large round colored sticker, red identifying them as possibly having flu. Green stickers signaled unlikely infection and orange stickers indicated other medical problems. As they moved on to triage, “patients” provided further information about symptoms such as coughing, high fever, body aches, and difficulty breathing that were likely flu-related. Some “patients” were “admitted” to the hospital. Others were “discharged” home.
Evaluators were stationed at every step of the way. They were charged with documenting adherence to hospital protocol. They noted, for example, whether “patients” and staff were wearing masks, if appropriate staff wore gowns, if chairs were regularly sanitized, and if spacing was properly maintained between potentially infectious “patients.” As an additional tool for evaluation, drill organizers recruited a professional video crew to document the disaster drill so that it could be carefully scrutinized following the event.
Arriving “patients” from a single family were cautioned to stay together. “Separation is a disaster,” said Michael Augenbraun, MD, Downstate’s director of infection control. He explained that in this kind of medical crisis, efforts are made to keep families together both to manage contagion and reduce anxiety. “Anytime there is exposure in the home, it’s highly likely everyone will get sick,” he said.
Both professional participants and volunteer patients were convinced of the usefulness of the exercise. “Drills are great,” said Tim Sheard, MA, RN, assistant director of infection control at Downstate. “This could happen. It’s like 911. It raises our awareness and allows us to find any gaps in out readiness plan.”
“Patient” Paul McNamee works in Child Immunization for the New York City Health Department. He said he found out about the drill through a friend. “I thought it would be a good experience,” said McNamee who coughed and complained of a temperature of 104 degrees, having fully thrown himself into the role. Nancy Hernandez, a pre-med student at CUNY’s Sophie Davis School of Biomedical Education, said, “I got an email from my dean and thought it would be interesting.”
Volunteers also included family members of Downstate staff. Clarence Bryant, environment health and safety specialist in the Emergency Department, for example, was on hand with his wife, son, daughter, and goddaughter. Bryant said the drill provided an opportunity for cooperation among staff members who might not normally work together. “The more interaction, the better they are able to interact. The more training, the better you are able to handle a real event,” said Bryant.